ORTHOPÄDIE A-Z
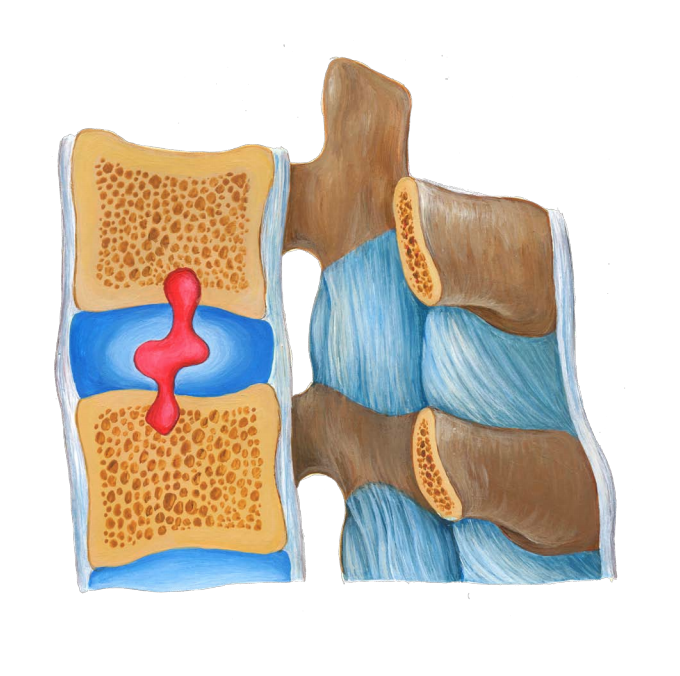
The outlook is generally favourable; the treatment, however, is time consuming(3–6 months). A reduction in discomfort can be achieved by a retraction of the herniatedvertebral disc and volume reduction, by cicatrisation or avoiding the nerve root in the bonyforamen. Complications resulting from the condition (cauda-syndrome, bladder and rectaldisturbances) are rare. An intervertebral disc surgery is necessary in only a few cases(approx. 10%) (discectomy, interlaminar windowing, sequestra removal, a combination ofdorsal intervertebral disc removal, reconstruction and replenishment of the intervertebraldisc area, in some cases with a stabilizing titan cage interposition, or implant of anartificial intervertebral disc).
In medical parlance as "popliteal cyst" or "synovial cyst" called. Thereis a swelling of the knee joint capsule back into the hollow of theknee. Its name comes from the first person to describe Dr. WilliamBaker, a surgeon from London (1877). Damage to meniscus orcartilage which is a long time, is handled by the body itself. Theresult is more synovial fluid to provide better gliding in theknee. If more synovial fluid formed, as mined, produced a kneejointeffusion. If the increase in synovial fluid long periods oftime, the joint capsule is expanding in order to provide thespace effusion. The point at which the knee joint capsule is theleast stable, is the knee, so that a bulge is formed into the hollowof the knee in chronic pressure. The Baker's cysts always makesdiscomfort when the pressure in the knee joint with increasedinflammatory activity or advanced cartilage damage increases. Thesurgical removal of the Baker's cyst is not useful if the cause - cartilage or meniscusdamage - persists.

Frequency:
A Baker's cystmay occurat any age, in principle. Children, however, are rarely affected by the formation of cystic changes in the popliteal fossa. Should, however, theformation of aBaker's cystin infancy, so boys are affected twice as often as girls. Mostly iti s possible the disease in middle and older age observed(40-60 of age).
Diagnostic imaging:
Magnetic resonance imaging (MRI Scan) to show the joint effusion,muscles, tendons, cartilage, menisci, cruciate and collateralligaments.
Therapy:
The individual consultation includes the behavior in everyday life, work and sport(avoiding knee burdensome sports). Medications, intraarticular injections with cortisone,physiotherapy, wearing a knee brace to stabilize and improvejoint function. The contents of the cyst can be sucked out bymeans of a puncture. With a recurrence of the cyst but canbe expected, because to describe it figuratively "thelake is pumped out, but the feeding flow continues".Under conservative measures is usually only comes toan improvement of symptoms caused by the Baker'scyst. A disappearance or "drying" of the cyst is notexpected. Only surgical treatment leads to adisappearance of the Baker's cyst.
The partial removal of the meniscusis the freedom from pain by removing all destroyed and mobile parts of the meniscus. Here,as much as possible should be maintained"healthy" meniscus tissue. The knee mirroring is carried out as part of an out patient surgery under local or general anesthesia. The surgical procedure will depend on the plan shape and the crack localization: All mobile fragments removed, smoothed there section margin, leaving a rimand the connection to the capsule, and flushed the joint.
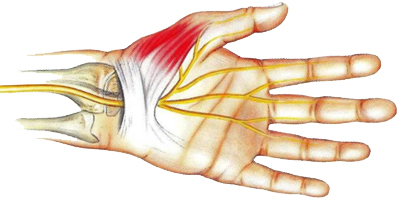
The Osteoarthritis of the hip is also known as degenerative arthritis,degenerative joint disease, or osteoarthrosis.It is a progressive destruction of articular cartilage underinvolvement of the bone, the joint capsule and the joint-surrounding musculature. Other causes include: metabolic diseases, accidents, infections, chronic congestion in sports or occupation, overweight, bands weaknesses, congenital malposition of the hip(dysplasia), hipdisordersin children(Perthes disease, epiphysiolysis) and/or int he course of inflammatory rheumatism. 10% of the population are affected. Often Coxarthrosisex is seven on both sides. Beginning in the 4th decade of life. Peak ageis 60 years. Sex ratio male : female=2 : 1
Symtoms:
Pain during exercise, increasing instability and Disabilities, limitations in walking distance, limping gait, crepitation, atrophy of muscles.
Diagnostic imaging:
X-ray of the hip joints in 2-3levels, pelvicradiograph: annulment, sclerosis of the joint space, bone attachments, cyst formation. Magnetic resonance imaging(MRI Scan) to show the muscles, tendons, cartilage and ligaments.
Therapy:
Reducing and avoiding overexertion and incorrect loading in everyday life, work and sport. Injections int he hip joint, concomitant drug treatment(anti-inflammatory, analgesic tablets). In the acute stage local refrigeration, in chronic stages of heat applications. Physiotherapy and manual therapy(mobilization, muscle stretching, eliminate muscle deficits, stabilize the thigh muscles),electrotherapy or acupuncture. Recently, the joint fluid replacement has well proven. It is restored by injection of synthetic hyaluronic acid, a new "joint lubricant".
Prognosis:
The course of the disease is usually progressive. Very often surgery is necessary. Joint-preserving surgery(corrective osteotomies of the femur, pelvis), or full or partial joint replacement(endoprosthesis). Cemented or uncemented implantation techniques. Individual planning of implants and materials to be elected. Autologous blood donation. Early postoperative mobilization, physical therapy, weight bearing, if necessary follow-up treatment. Increased wareness of seats, allowing movement and resilience. Regular postoperative clinical and radiological controls.
![]()
It is an acquired painful irritation in the area of the elbow at theorigin of the tendons. If the area of the external upper arm isinflamed, this is called epicondylitis humeri radialis or "tenniselbow". If the inner upper arm is affected, this is calledepicondylitis humeri ulnaris ("golfer's elbow"). Typically, there is animbalance between mechanical activity (one-sided strain, highphysical activity) and reduced load capacity of the biologicalstructures (extensor tendon attachments on the elbow). Inmost cases there is chronic overloading of the arm (PCactivity, keyboard use).
Symptoms:
local pressure pain in the area of the tendonattachment of the elbow. Provocation of pain by stretchingthe elbow against resistance. Reduction of thestrength of the arm or hand. Restriction of theforearm turning movements.
Therapy:
Information about the disease, its naturalcourse and the treatment options. As a rule, areduction in physical activity for a limited period oftime (certificates, sports exemption), as well aswearing a special elbow joint brace or epicondylitis brace iscompletely sufficient. Further measures are manual therapy(stretchingexercises, transverse friction), medicinal ointment applications, iontophoresis, targetedcorticoid injections or acupuncture. In the acute stage local cold applications, in chronicstages heat applications.
Prognosis:
The Epicondylitis almost heals without consequences. Extracorporeal shockwave therapy (ESWT) is successful (66%) for persistent, chronic diseases. Only in isolatedcases is an outpatient operation necessary (notching of the extensor tendons close to theirorigin according to Hohmann, denervation at the Epicondylus according to Wilhelm).
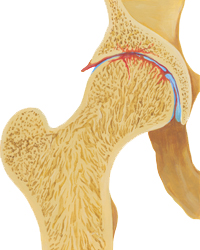
Reduction, avoiding over exertion and incorrect loading in everyday life, work and sport. First, gentle load design, dodging on sports that do not burden the affected heel region: egcycling, swimming, etc. Localice treatment, ultrasound, physiotherapy and manual the rapyin the area of the plantarfascia (crossfriction).Anti-inflammatory medications are injected into the painful area(injection of corticosteroids), wearing silicone heel pador shoe insoles.
The course of the disease is usually favorable, severe progressive forms are rare. When achieved freedom from paina gradual, slow load structure is essential. The sport-specific load or partload can take place only if it is possible under an algesia. In stubborn cases, extracorporeal shockwave therapy is helpful. Surgery isa last resort, here the tendon plate of the sole(plantar fascia) is severed and removed the bony heel spur.
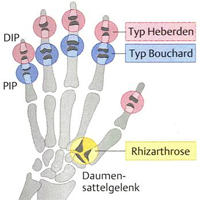

The course of the disease is benign. Only in individual cases is an operation(finger joint stiffening, so called arthrodesis in function position) necessary. In principle, open methods are used. Swelling and pain usually disappear rapidly after surgery.Recurrences may occur.

The treatment of acute gout consists in immobilization, cooling and administration of plant(colchicine) oranti-rheumatic drugs(etoricoxib). The prophylaxis of gout are dietary measures(avoidance of legumes and meats, especially organ meats) and the reduction of alcohol consumption, especially beer! If gout is not relieved by these measures, a continuous administration of medications is necessary to permit the formation of uric acid in the body decrease(allopurinol, febuxostat).
The course of the disease is usually favorable, severe progressive forms are rare. The individual advice includes eating behavior and alcohol consumption in everyday life. Accompanying measures such. As weight reduction, regular physical activity. Gout is subject to regular medical check(blood draws: uric acid levels) and an intensive, long-term treatment.

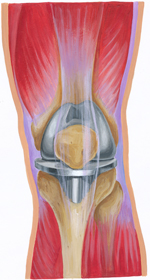
The course of the disease is usually progressive. Very often surgery is necessary. Joint-preserving surgery(femoral ortibial plateau corrective osteotomies) or the complete or partial joint replacement(endoprosthesis). Individual planning of implants and materials to be elected. Autologous blood donation. PostoperativePhysiotherapy, early mobilization and weight bearing. Clarification of allowable movements and resilience. Regular clinical and radiological follow-ups.


The aim is the correction of the malposition, pain relief, functional gain and improved aesthetics. joint-preserving surgery, for example surgical methods for Chevron, Austin or Scarf(removal of pseudoexostosis, soft tissue work on the capsule and the muscle attachment, corrective osteotomy, possibly simultaneous surgical correction of the deformity of adjacent toes, so called hammer toe orc law toe). Treatment means after-surgery shoe for a period of4-6weeks. When achieved freedom from pain a

1 - occipital pain, stiff neck
2 - discomfort, muscle tension, Disabilities
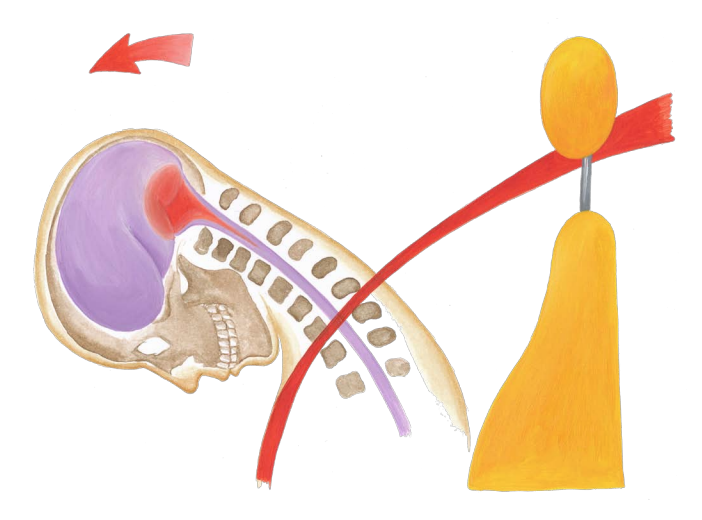
The course of the disease is low. Usually you go - with all severities of whiplash -from a regression period of about 3-6 weeks from. Only about 10% of patients, the symptoms expand over a period of 6 months. Late effects due to a whiplash injury are rare.Studies have shown that only a very small percentage of about 2-3% still have symptoms two years after the injury.
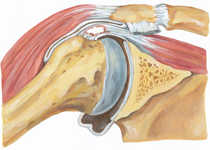
It is a painful inflammation of a bursa with or without calcification in combination with a wear (degeneration) oft end on tissue. The rotator cuff of the shoulder joint dislocated in a narrow tendon channel of the bony corner articulation (acromion) and the humeral head (humerus) is limited. The swollen tendons rub on movement in the anatomically narrow space and thus it comes to inflammation("impingement syndrome"). In up to 90% of the supraspinatus tendon is affected. The acutes houlder pain preferably occurs in younger and active patients. Symptom is a dull, dragging pain in the deltoid region. Shoulder movements over 90degrees are hardly possible. Chronic shoulder pain leads to posture and atrophy of the muscles. The peak age is 35-50 years. Sex ratio women : men = 2 : 1.
In the acute stage, only the targeted injection of an anti-inflammatory pain medication is usually helpful. In addition, physiotherapy and manual therapy for mobilization and strengthening the shoulder muscles. Other measures include electrotherapy, cold applications or acupuncture. The individual consultation includes the behavior in everyday life, the physical strain at work and in sports(avoidance of overhead work, sports with heavy use of the shoulder joints).

The course of the disease is usually favourable, severe forms of the disease are rare. Only in isolated cases is surgery(arthroscopy, possibly acromioplasty) necessary.
Pain relief or reduction. Removing any existing neurological symptoms. Physiotherapy and manual therapy to strengthen the abdominal and back muscles and to maintain the mobility of the affected spinal segments. In recent years the so-called Periradicular Therapy(PRT) under Cat Scan guidance (Computertomography) is very successful. Other treatment measures are heat
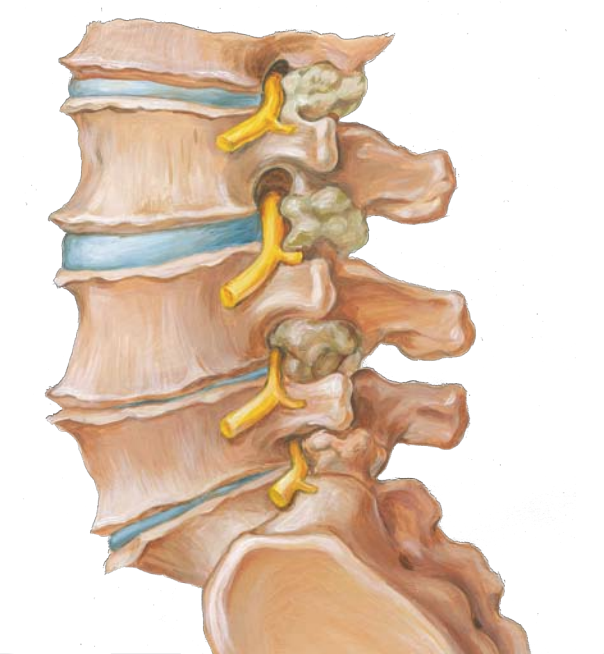
The course of the disease is usually low, heavy progressive forms are rare.Education about the disease, its natural history and its ability to influence by conservative or surgical treatment. Assistive devices(corset bodice, back brace with velcro). Only in rare cases is a surgery(decompression, different extent and location, possibly additionally instrumental in stabilizing method of existing or expected instability) is necessary.


The partial removal of the meniscus is the freedom from pain by removing all destroyed and mobile parts of the meniscus. Here, as much as possible should be maintained"healthy" meniscus tissue. The knee mirroring is carried out as part of an out patient surgery under local or general anesthesia. The surgical procedure will depend on the plan shape and the crack localization: All mobile fragments removed, smoothed the resection margin, leaving arimand the connection to the capsule, and flushed the joint.
The mainstay of therapy are anti-inflammatory drugs such as ibuprofen, phenylbutazone, diclofenac, indomethacin, naproxen and COX-2 inhibitors. Disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine, methotrexate, local injection with corticosteroid. Tumor necrosis factor-alpha (TNFα) blockers, such as the biologic set an ercept, infliximab, golimumab and adalimumab. Physiotherapy to strengthen
education about the disease, its history and its ability to influence episodic by a modern, individual therapy. The course of the disease is usually low, severe progressive forms are rare.
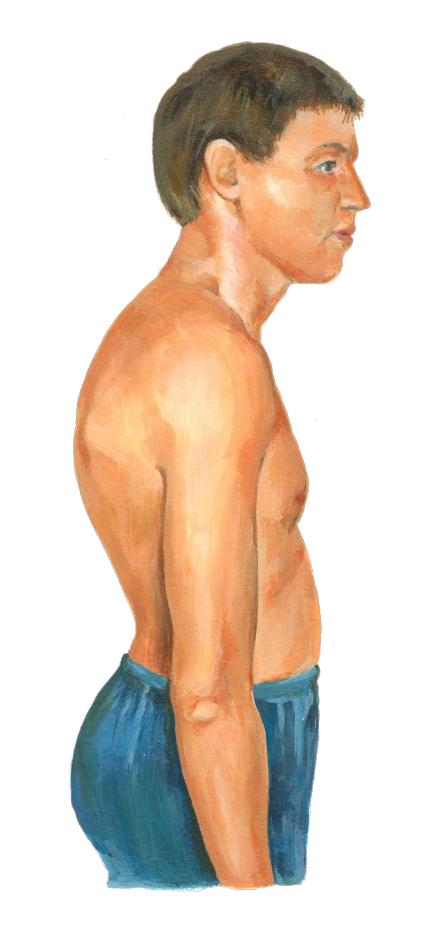
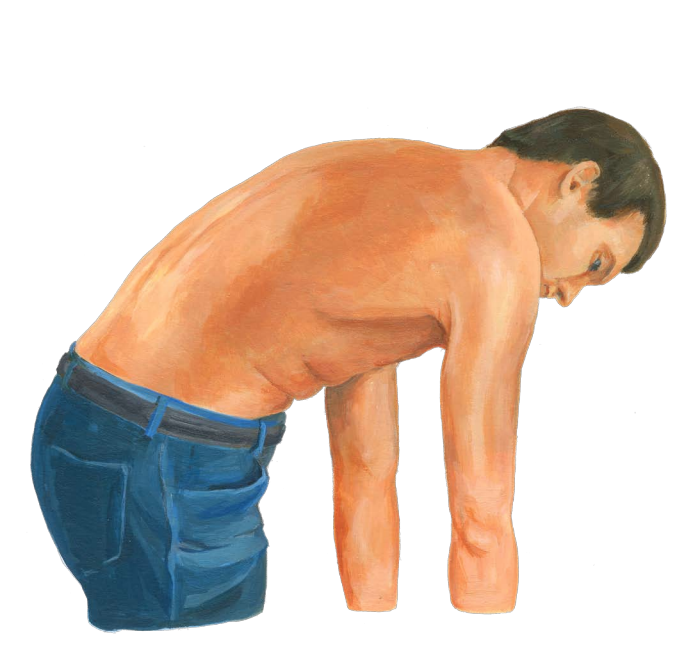
The course of the disease is usually low, severe progressive forms are rare. Only in severe during puberty is sometimes aback brace(at bends from45 degrees: Milwaukeeor Bostoncorset) or surgery(fixed kyphos is at adult skeleton from an angle of60 degrees, a combination of aventraldisc nucletomy, erection and fill the intervertebral discspace by own bone with a dorsal stabilization) required.
targeted antibiotic therapy with proven or very likely still persistent infection. Asa causal therapy is not possible(NSAIDs, Coxibs) is treated symptomatically withanti-inflammatory drugs. In chronic disease conditions initiation of a drug Rheumatism based therapy (Sulfasalazine, MTX, Biologica).
the course of the disease is low, the duration of treatment, however, rather tedious(Ø =3-15months). Healing in 80% of cases within 3-6 months. However, severe progressive form sorachronic course(about 10%) are possible.
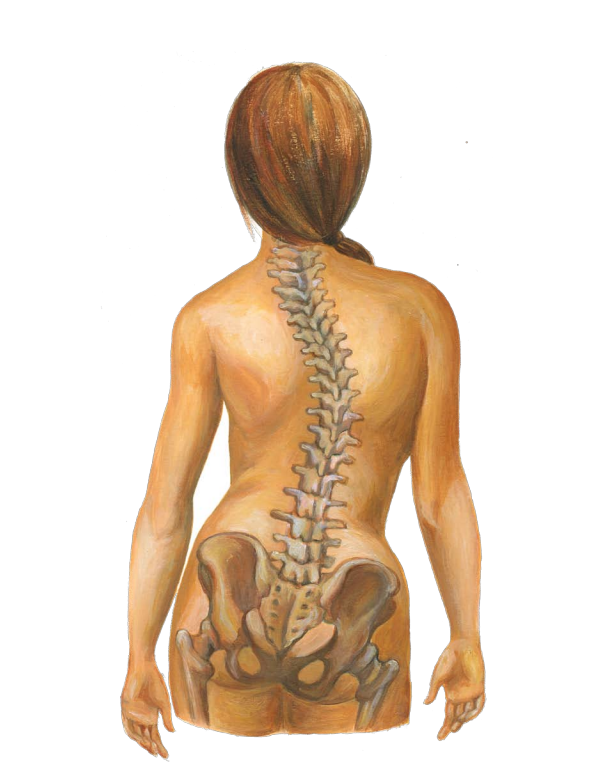
The course of the disease is usually low, severe progressive forms are rare. The scoliosis requires regular medical checks and an intensive, long - term treatment. Only in rare cases is aback brace(Milwaukee or Boston corset) or possibly an operation(fixed scoliosis from an angle of 40degrees, a combination of aventral disc surgery, erection and filling of the intervertebral disc space by own bone with aventral ordorsal stabilization)necessary. After completion of growth, there is usually no significant findings deterioration.
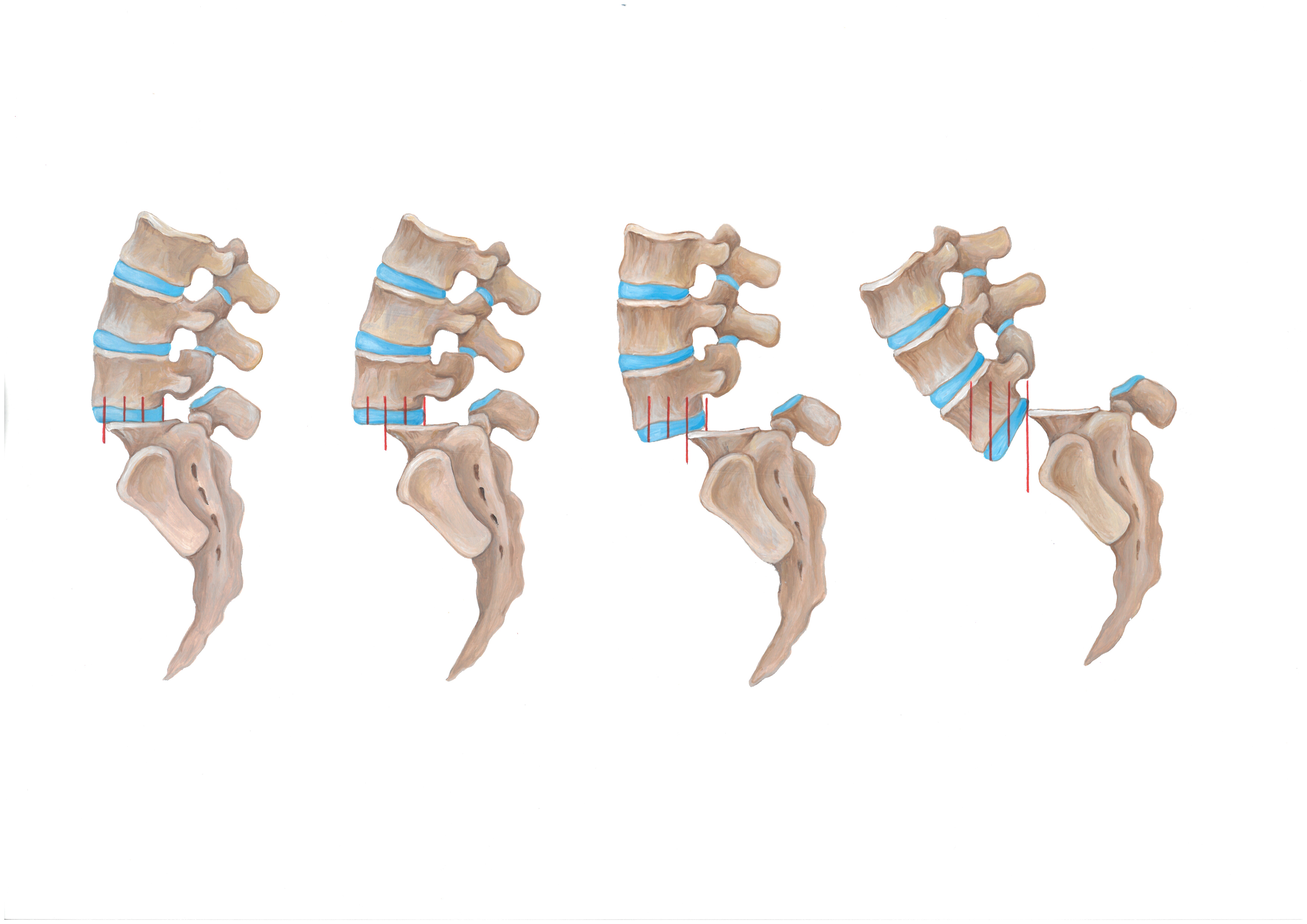
The course of the disease is usually low, heavy progressive forms are rare. The sliding operation can spontaneously come to a halt at any stage. With increasing sliding the likelihood of complaints, dysfunction and neurological symptoms increases. Aids